
By Melissa Flores, California Health Report
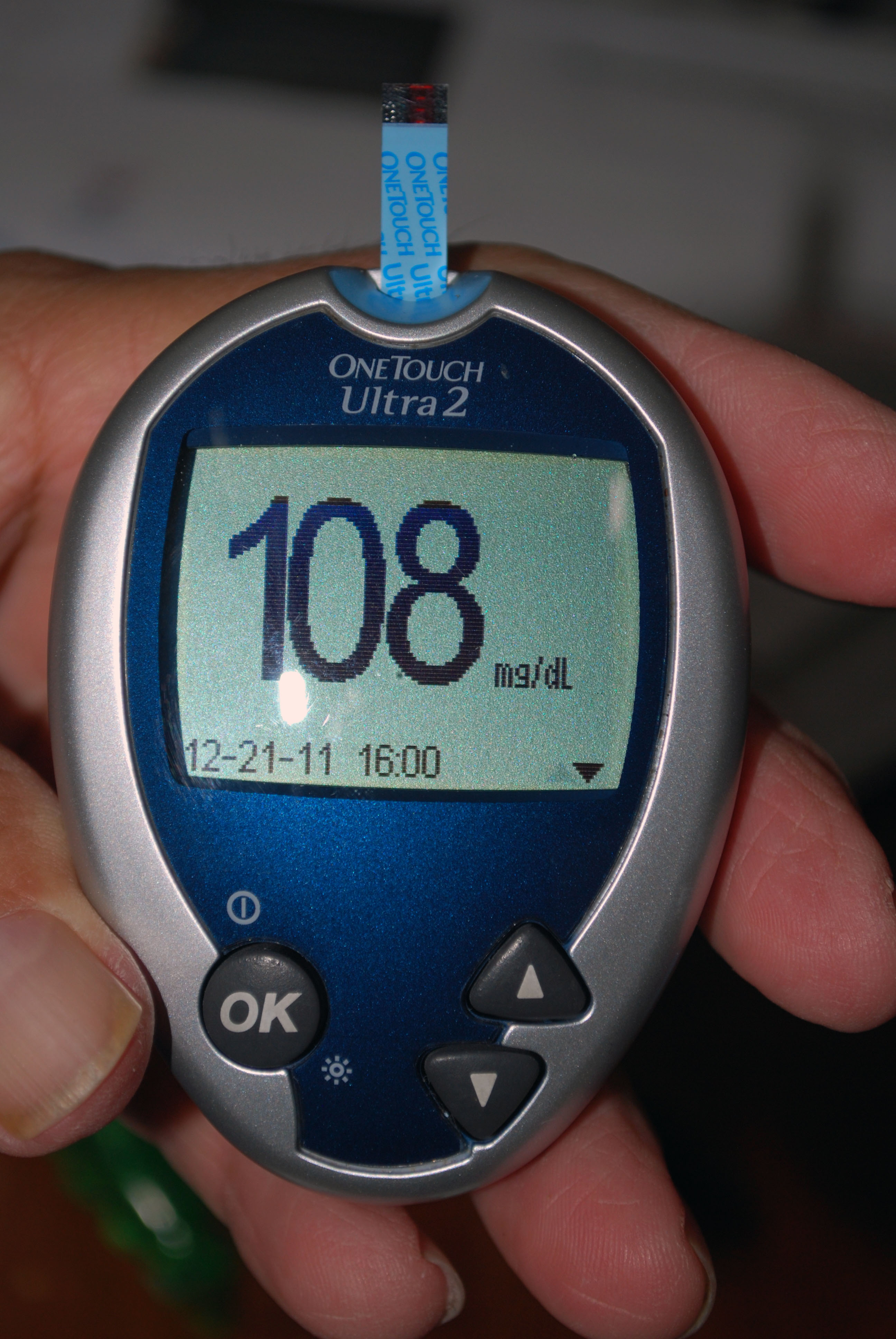
When a patient is admitted to the Community Hospital of the Monterey Peninsula, staff members always run a quick test for blood sugar levels.
The rate of diabetes in Monterey County, which includes Salinas, is 8.1 percent, according to the most recent figures from the California Diabetes Program. A community health survey found that 9.8 percent of adults in the service area of Community Hospital have been diagnosed. But about 18 percent of patients admitted for treatment at the hospital have diabetes.
The hospital, which services cities from around the central coast including Salinas, recently received a gold seal of approval from the Joint Commission for its advanced inpatient diabetes care. It is one of six hospitals to receive the certification in California, and one of 41 in the nation. The Joint Commission is an independent, nonprofit that accredits and certifies more than 19,000 health care organizations or programs in the United States.
“We are following the American Diabetes Association guidelines for common things,” said Christine Short, a registered nurse and a quality management analyst, of the checklist that staff uses to provide the best care.
“We have every reason to believe that diabetes rates will continue to rise,” said Debra Simonian, a registered dietician and clinical nutrition manger. “Standardizing care will increase patient outcomes.”
Patients at Community Hospital, which is a 30-minute drive from Salinas, are sometimes admitted for complications due to diabetes. Short said that 20 percent of patients with diabetes are admitted for a complication. Other patients are admitted for an unrelated illness for which hospital staff needs to take the condition into account.
“We look at all the high and low blood sugars,” said Short, of testing all patients who are admitted to the hospital. “We can spot anyone who doesn’t have a diagnosis who needs to be looked at, system wide.”
A low or high blood sugar can cause complications such as infections or cardiovascular complications, slower healing time and other issues that lead to longer hospital stays.
The staff also tests A1c levels, a test that can look at how a diabetic patient has controlled his or her blood sugar over a three-to-six-month period. Nurses and doctors know that if the patient has an A1c level of 7 percent or more, which looks at sugar levels in the hemoglobin, the patient’s blood sugar may be harder to control or the patient may have more complications.
Short said another of the changes the hospital has made is that inpatients are given insulin instead of oral medications. Medication is also coordinated with meal time to help maintain a steady blood sugar level in patients.
“In the published literature, it says it’s a better way to manage it,” Simonian said, of switching patients on oral medication to insulin for the duration of the stay. “It is more predictable.”
Short said the staff is trained to explain to patients why they are taken off oral medications and using insulin instead – and they are told that they will be able to continue with their oral medications when they return home.
“We do a lot of patient education on it,” she said.
“Part of the certification process is a lot of education of physicians, staff, as well as to patients,” Simonian said.
Patients who are diabetic are provided with low-carb meal options for their in-hospital meals.
“We work closely with physicians in terms of diet,” Simonian said, noting that they take into consideration other conditions such as kidney disease or high blood pressure that might also influence diet.
The staff members are trained to give patients with diabetes a Diabetes Survival Skills packet, available in English or Spanish. It explains to patients how to handle the illness once they are released, such as testing their blood sugar at home. The hospital can also refer patients to a variety of services such as classes on diabetes, nutrition or support groups.
With newly diagnosed patients, a patient educator would meet with them immediately to cover resources that are available to learn about diabetes and to offer support.
“We handle it in the hospital,” Simonian said. “They may be referred to outpatient services (after they are released) if they are newly diagnosed.”
Short added that it is a high priority to see the patients before they leave the hospital to talk about what a diabetes diagnosis means and what resources are available.
The staff members who participated in the certification process included an interdisciplinary group of physicians, pharmacists, patient educators, lab technicians and ancillary staff, such as those who deliver meals or housekeepers.
Short said that the complete list of guidelines went into effect in September and they have been monitoring data to see if they have improved the outcome. She said it is too early to tell if patient stays have shortened, but they have seen that all patients are being checked for their blood sugar levels and A1c levels.
“When Community Hospital decides to go under scrutiny, we only do it when there is clear clinical merit that is evidence based, as well as operational standards, “said Brenda Moore, communications and marketing assistant director for Community Hospital. “It has to have both those features.”
Members of the Joint Commission came to the hospital in December to do a rigorous on-site survey to evaluate compliance with the standards.
“In achieving Joint Commission certification, Community Hospital has demonstrated its commitment to the highest level of care for its patients with diabetes,” said Jean Range, the executive director of Disease-Specific Certification for the Joint Commission. “Certification is a voluntary process and I commend Community Hospital for successfully undertaking this challenge to evaluate its standard of care and instill confidence in the community it serves.”
Moore said the hospital undertook a similar certification with the Joint Commission for dealing with stroke victims.
“The Joint Commission helps with a way to implement it,” Simonian said.
“The incidence of diabetes is growing at an alarming rate here and across the country,” said Steven Packer, the president and CEO of Community Hospital, in a press release. “This certification demonstrates Community Hospital’s commitment to excellence in providing care to patients who have this disease or may be at risk for it.”
Melissa Flores is a correspondent for the California Health Report at www.calhealthreport.org






You must be logged in to post a comment.